Med-Fit Tech Assistant
Human Anatomy - Learning Module #4
The Cardio-Pulmonary-Vascular System
Part A
Part A: The Cardiac System
Learning Objectives:
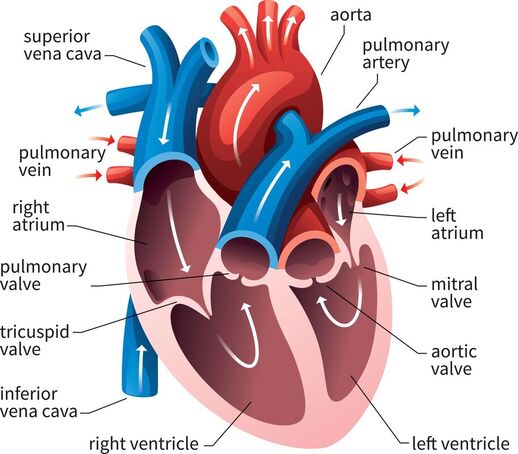
The heart is a specialized muscle that functions as a mechanical pump. Each contraction develops pressure and ejects blood into the pulmonary and peripheral vascular systems of arteries and veins. The pulmonary system oxygenates the blood with each breath, and the peripheral system delivers oxygen continually to all 50-100 trillion cells of the human body.
The heart has 4 chambers: an atrium and a ventricle on each side of the heart, right and left. Each side functions as a separate pump. One-way valves between these chambers direct the blood flow under pressure with each contraction of the heart.
The Circulation of Blood through the Heart
The peripheral vascular system returns de-oxygenated blood to the heart by converging into the superior vena cava (blood from the veins of the upper body) and the inferior vena cava (blood from the veins of the lower body). Both vena cavae empty into the right atrium.
The right atrium pumps the blood through the tricuspid valve into the right ventricle.
The right ventricle pumps the blood through the pulmonary valve into the pulmonary artery to go to the lungs for oxygenation.
The oxygenated blood from the pulmonary system returns to the heart by converging into four pulmonary veins. All four pulmonary veins empty into the left atrium.
The left atrium pumps the blood into the left ventricle through the mitral (bicuspid) valve.
The left ventricle pumps the blood through the aortic valve into the aortic artery (aorta), which supplies the peripheral vascular system with oxygenated blood.
Learning Objectives:
- Describe the structure of the heart
- Describe the path of blood through the heart
- Describe the unique characteristics of cardiac muscle
The heart is a specialized muscle that functions as a mechanical pump. Each contraction develops pressure and ejects blood into the pulmonary and peripheral vascular systems of arteries and veins. The pulmonary system oxygenates the blood with each breath, and the peripheral system delivers oxygen continually to all 50-100 trillion cells of the human body.
The heart has 4 chambers: an atrium and a ventricle on each side of the heart, right and left. Each side functions as a separate pump. One-way valves between these chambers direct the blood flow under pressure with each contraction of the heart.
The Circulation of Blood through the Heart
The peripheral vascular system returns de-oxygenated blood to the heart by converging into the superior vena cava (blood from the veins of the upper body) and the inferior vena cava (blood from the veins of the lower body). Both vena cavae empty into the right atrium.
The right atrium pumps the blood through the tricuspid valve into the right ventricle.
The right ventricle pumps the blood through the pulmonary valve into the pulmonary artery to go to the lungs for oxygenation.
The oxygenated blood from the pulmonary system returns to the heart by converging into four pulmonary veins. All four pulmonary veins empty into the left atrium.
The left atrium pumps the blood into the left ventricle through the mitral (bicuspid) valve.
The left ventricle pumps the blood through the aortic valve into the aortic artery (aorta), which supplies the peripheral vascular system with oxygenated blood.
The muscular walls of the different heart chambers differ according to the amount of pressure against which they pump:
Many diseases cause increased resistance in the peripheral vascular system, which can greatly increase blood pressure. High blood pressure over time can damage the heart, the arteries of the vascular system, and even some ends organs, such as the brain, kidneys, and eyes.
Cardiac muscle shares a few characteristics with both skeletal muscle and smooth muscle, but it also has some unique properties of its own. Contractions of the heart (heartbeats) are controlled by specialized cardiac muscle cells called pacemaker cells that directly control heart rate. This property is known as autorhythmicity. (Neither smooth nor skeletal muscle can do this.)
Although cardiac muscle cannot be consciously controlled, the pacemaker cells respond to signals from the autonomic nervous system (ANS) during periods of rest, exercise, or stress to either speed up or slow down the heart rate. The pacemaker cells can also respond to various hormones that modulate heart rate and blood pressure.
There are two major types of cardiac muscle cells:
The function of myocardial conducting cells is similar in many ways to neurons, although they are specialized muscle cells. Myocardial conduction cells initiate and propagate the action potential (the electrical impulse) that travels throughout the heart muscle and triggers the cardiac muscle contractions that propel the blood.
A “normal” heart rate at rest ranges between 60 and 100 beats per minute depending on a variety of factors. In certain diseased states, the heart rate can exceed 100 (tachycardia). When a person is healthy and more physically fit than normal, the resting heart rate tends to be in the lower range of normal or even below 60 (bradycardia).
During strenuous exercise, the oxygen demands of the heart and skeletal muscles cause the autonomic nervous system to increase the heart rate to match the demand. A person’s maximum heart rate decreases with age. A basic formula for calculating a person’s predicted Maximum Heart Rate (MHR) is: 220 – Age = MHR.
- The walls of the right atrium and ventricle are thin compared to the walls of the left atrium and ventricle, because the right side of the heart pumps into the pulmonary vascular system which is a very low pressure system.
- The walls of the left atrium and ventricle are thick compared to the walls of the right atrium and ventricle, because the left side of the heart pumps into the peripheral vascular system which is a high pressure system.
Many diseases cause increased resistance in the peripheral vascular system, which can greatly increase blood pressure. High blood pressure over time can damage the heart, the arteries of the vascular system, and even some ends organs, such as the brain, kidneys, and eyes.
Cardiac muscle shares a few characteristics with both skeletal muscle and smooth muscle, but it also has some unique properties of its own. Contractions of the heart (heartbeats) are controlled by specialized cardiac muscle cells called pacemaker cells that directly control heart rate. This property is known as autorhythmicity. (Neither smooth nor skeletal muscle can do this.)
Although cardiac muscle cannot be consciously controlled, the pacemaker cells respond to signals from the autonomic nervous system (ANS) during periods of rest, exercise, or stress to either speed up or slow down the heart rate. The pacemaker cells can also respond to various hormones that modulate heart rate and blood pressure.
There are two major types of cardiac muscle cells:
- Myocardial contractile cells constitute the bulk (99%) of the cells in the atria and ventricles. Contractile cells conduct impulses and are responsible for contractions that pump the blood through the body.
- Myocardial conducting cells (1% of the cardiac cells) are the autorhythmic cells and form the conduction system of the heart. These are much smaller than the contractile cells (except for the Purkinje conducting cells of the heart) and have few of the myofibrils or filaments needed for contraction.
The function of myocardial conducting cells is similar in many ways to neurons, although they are specialized muscle cells. Myocardial conduction cells initiate and propagate the action potential (the electrical impulse) that travels throughout the heart muscle and triggers the cardiac muscle contractions that propel the blood.
A “normal” heart rate at rest ranges between 60 and 100 beats per minute depending on a variety of factors. In certain diseased states, the heart rate can exceed 100 (tachycardia). When a person is healthy and more physically fit than normal, the resting heart rate tends to be in the lower range of normal or even below 60 (bradycardia).
During strenuous exercise, the oxygen demands of the heart and skeletal muscles cause the autonomic nervous system to increase the heart rate to match the demand. A person’s maximum heart rate decreases with age. A basic formula for calculating a person’s predicted Maximum Heart Rate (MHR) is: 220 – Age = MHR.
Learning Module 4A: LAB
1. Recite the course of blood through the heart by naming the different structures in order.
2. What is the most unique characteristic of cardiac muscle?
3. Calculate your predicted MHR.
4. Watch a YouTube video on how to measure your heart rate at your wrist or neck. Then measure your heart rate (beats per minute) when at rest. Measure your heart rate again immediately after a strenuous activity, such as: running a quarter mile or taking several flights of stairs.
Extra Credit: Continue taking your post-exercise heart rate every half-minute x 4 to see how quickly your heart rate returns to your resting heart rate. (A quicker recovery indicates a higher level of fitness.)
2. What is the most unique characteristic of cardiac muscle?
3. Calculate your predicted MHR.
4. Watch a YouTube video on how to measure your heart rate at your wrist or neck. Then measure your heart rate (beats per minute) when at rest. Measure your heart rate again immediately after a strenuous activity, such as: running a quarter mile or taking several flights of stairs.
Extra Credit: Continue taking your post-exercise heart rate every half-minute x 4 to see how quickly your heart rate returns to your resting heart rate. (A quicker recovery indicates a higher level of fitness.)